Jennifer McQuiston isn’t worried about her children getting kisses from the family’s dogs.
The recent reports of death and serious injury to two Wisconsin residents tied to bacteria in dogs' saliva is no reason to panic, McQuiston said.
Why should anyone care what McQuiston thinks?
She’s one of the nation’s leading experts on capnocytophaga, the bacteria at the center of the tragedies.
“I have two dogs and they play and lick my children every day, and I am not concerned about capnocytophaga, (pronounced cap-no-sa-TOE-faga)” said McQuiston, deputy director of the Division of High-Consequence Pathogens and Pathology with the federal Centers for Disease Control and Prevention in Atlanta.
More important is recognizing the symptoms of sepsis — a potentially life-threatening complication of an infection — and getting immediate medical attention, she and other experts said.
“What’s really happening is a rapidly overwhelming bacterial infection,” McQuiston said.
And typically, if recognized early and the person has no underlying health problems, capnocytophaga will respond to penicillin or another common antibiotic.
“In the vast majority of cases, people do not get sick from this,” she said.
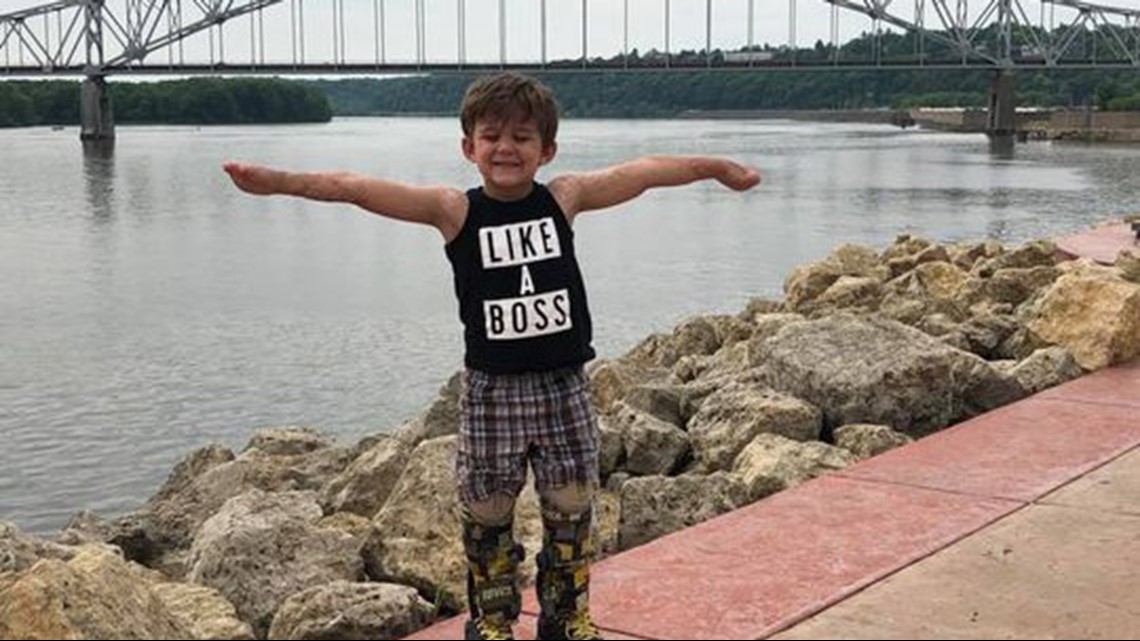
The bacteria led to the June 23 death of Sharon Larson, 58, of South Milwaukee woman and the June amputation of the hands and parts of the legs of Greg Manteufel, 48, of West Bend. In 2015, a 3-year-old Liam Young of Louisburg had to have his fingers and toes amputated after he developed the same kind of infection.
The CDC does not track the number of cases of illness from capnocytophaga — states have not made it a requirement to report such infections to the CDC — but the agency is confident illness from the bacteria is rare.
The CDC has confirmed nine cases since 2015. However, agency officials admit they don’t know the full scope because labs across the USA are able to test and confirm the bacteria, meaning not all samples are sent to the CDC.
The two recent Wisconsin cases were not sent to the CDC. The CDC learned about them from media reports and reached out to the Wisconsin Health Department.
CDC officials also get an indication of the infection's prevalence by looking at the agency's MicrobeNet database that doctors and hospitals use to research rare bacteria. In the past year MicrobeNet has received 12 reports of capnocytophaga infections, McQuiston said.
According to the CDC, 74% of dogs have capnocytophaga detected in their mouths, and about 36% of the U.S. population owns at least one dog.
“There are so many dogs and so many people and interactions with dogs, that tells you how rare this is," she said. "Pets play a really important part of human existence.
“The answer is not to get rid of your pet or test your dog.”
Illness follows puppy bite
On a normal Tuesday evening, Sharon and Daniel Larson were visiting with their son and daughter-in-law. It was about 5 p.m. when their Shih Tzu puppy nipped Sharon's finger — just a nip, nothing that seemed serious.
The following evening, Sharon Larson felt as if she were getting the flu. She began throwing up the next morning.
Her husband chided her to go to the doctor when she told him she wasn’t going to work that morning, but Sharon Lawson told him she would sleep it off. By about noon, he noticed his wife was pale, according to their son, Steven Larson.


He drove her to Urgent Care at Wheaton Franciscan Healthcare. Taking one look at Sharon Larson, doctors told them to go to the emergency room.
They took her vital signs and discovered that her blood pressure was extremely low, so low that doctors were surprised she was still alive, her son said.
Doctors recognized the signs of sepsis and administered antibiotics immediately. Family mentioned all the factors they thought might be relevant: the dog bite, a visit to her daughter in Colorado the week prior, her work at a bank where she often handled money.
Doctors weren’t sure what was causing what appeared to be a serious infection. In addition to the antibiotics,they ran ultrasounds, took X-rays, performed an emergency CT scan, took cultures of her blood. Sharon Larson continued to worsen.
By 1 a.m. Friday, she began showing signs of organ failure.
Doctors sedated her and put her on a breathing tube and dialysis. Her condition became grave.
Four days after the dog bite, she died. Doctors did not find out until later that what killed her was capnocytophaga though they had suspected it.
“My mom was 58 years old, and she had dogs all her life," Steve Larson said Monday. "They licked and nibbled her, and she was fine — until the last four days of her life.”
Steven Larson said they will remember their mother as a kind, genuine person who loved her family, her pets, her bank job and life itself.
"She was a great person," he said. "I know I can't change anything; I can't bring my mom back. But if I can help another family hold onto their loved one by sharing this story, I'll do that."
Sneaky bacteria

Capnocytophaga bacteria living in animals' mouths are common and crafty, according to experts.
The reasons dogs and cats are able to live with the bacteria is because it is part of their microbiome, or community of microbes. Humans have their own, different communities of microbes.
"This organism has developed some tricks to evade immune responses," said Christopher W. Olsen, a professor emeritus of public health at the University of Wisconsin-Madison School of Veterinary Medicine.
The bacteria are able to evade white blood cells called macrophages and also have the ability to enter the body without triggering the signaling system that normally alerts the body to foreign organisms, Olsen said.
Although people tend to think of large bites or wounds a gateway to capnocytophaga, Olsen stressed that the bacteria can enter the body through relatively small cuts or fissures in the skin.
"I dare say the average practicing doctor has never heard of this bacteria," said William Schaffner, a professor of preventive medicine and infectious disease at Vanderbilt University Medical Center in Nashville, Tennessee. "It's not reportable. We, as doctors, just know it is pretty darned unusual."
Schaffner said the bacteria are often found in dog and cat saliva "and on occasion, you can even find this bug in human saliva."
When the bacteria find their way into unusual niches, they can wreak havoc.
When capnocytophaga get beneath human skin, they find a rich environment of nutrients in our fatty and fibrous tissue. These nutrients allow the bacteria to multiply rapidly.
The danger increases significantly if the bacteria get into the bloodstream. This can happen in the case of a dog bite or any wound that has damaged blood vessels.
Infection is more likely to result from the bite of a dog than from a cat, Schaffner said. Dog bites are crushing injuries that carry a higher probability of damaging blood vessels.
Humans most vulnerable to the bacteria include alcoholics, older adults, people with weakened immune systems and those lacking a spleen. The spleen acts as an effective filter for the blood and fights certain kinds of bacteria.
Alcoholics are at greater risk from the bacteria because they have less efficient infection-fighting white blood cells.
However, the Wisconsin victims were not compromised in these ways.
Once the bacteria enter the bloodstream, they trigger an inflammatory response that results in such symptoms as high fever and shock.
Early signs of a human infection from the bacteria include redness, swelling, a discharge, puffiness and pain.
Long recovery road
Manteufel of West Bend is still undergoing treatments at Froedtert Hospital in Milwaukee for the infection he contracted in June.
His case is atypical: No dogs or cats bit or scratched him, and he didn’t have any health conditions that would predispose him to infection.
His prior medical history consisted of a sprained ankle and not much more, said his wife, Dawn.


If Greg Manteufel had been an alcoholic, he probably wouldn’t be alive today, his wife said doctors told her.
His flu-like symptoms first appeared the evening of June 25 with a fever and vomiting that worsened over the next day. By the night of the 26th, family members say he was delirious, talking gibberish, and had severe leg pain but insisted on lying back down instead of going to the hospital.
By the time he got to the hospital at 5:30 the next morning, he was turning black and blue as blood vessels began to burst all over his body.
Doctors started him on antibiotics immediately and initially asked questions about his exposure to ticks and spiders. They sent his blood samples out of state for testing.
The capnocytophaga diagnosis didn’t come for eight days. He has lost parts of all four limbs to sepsis and will require reconstructive surgery on his nose.
This week he is having his ninth surgery. He is expected to have at least 11 surgeries total before moving to rehab and recovery in coming weeks.
What you need to know
Question: Should pet owners be worried about a dog lick?
Answer: Experts with the federal Centers for Disease Control and Prevention say pet-owners should not panic. Infections from capnocytophaga are extremely rare. Jennifer McQuiston, one of the nation's leading experts on the bacteria with the CDC, has two family dogs and lets them play with and lick her children every day.
Q. What should someone do if they get a dog bite?
A. If a dog or cat bit you, call your doctor right away even if you don’t feel sick. Animal bite wounds should be washed immediately and thoroughly with soap and water.
Talk to your doctor about the possible need for antibiotic treatment and a tetanus vaccination.
Q. What symptoms suggest a dog or cat bite may be infected?
A. If the bite area develops redness, swelling, puffiness, pain or a discharge, seek medical help right away.
Q. What is sepsis and how do doctors treat it?
A. Sepsis is a potentially life-threatening complication of a local infection. Your immune system generally protects you, but it can go into overdrive and lead to severe inflammation throughout your body.
Symptoms include fever, high heart and respiratory rates and abrupt change in mental state. Treatment is often an aggressive regimen of antibiotics.
Source: U.S. Centers for Disease Control and Prevention, Wisconsin Health Department, infectious disease experts