CLEVELAND — When the world lost actor Chadwick Boseman in August, his death from colon cancer exposed a troubling trend: the mysterious rise of cases in otherwise healthy, young men. Even more alarming: black men are even more at risk.
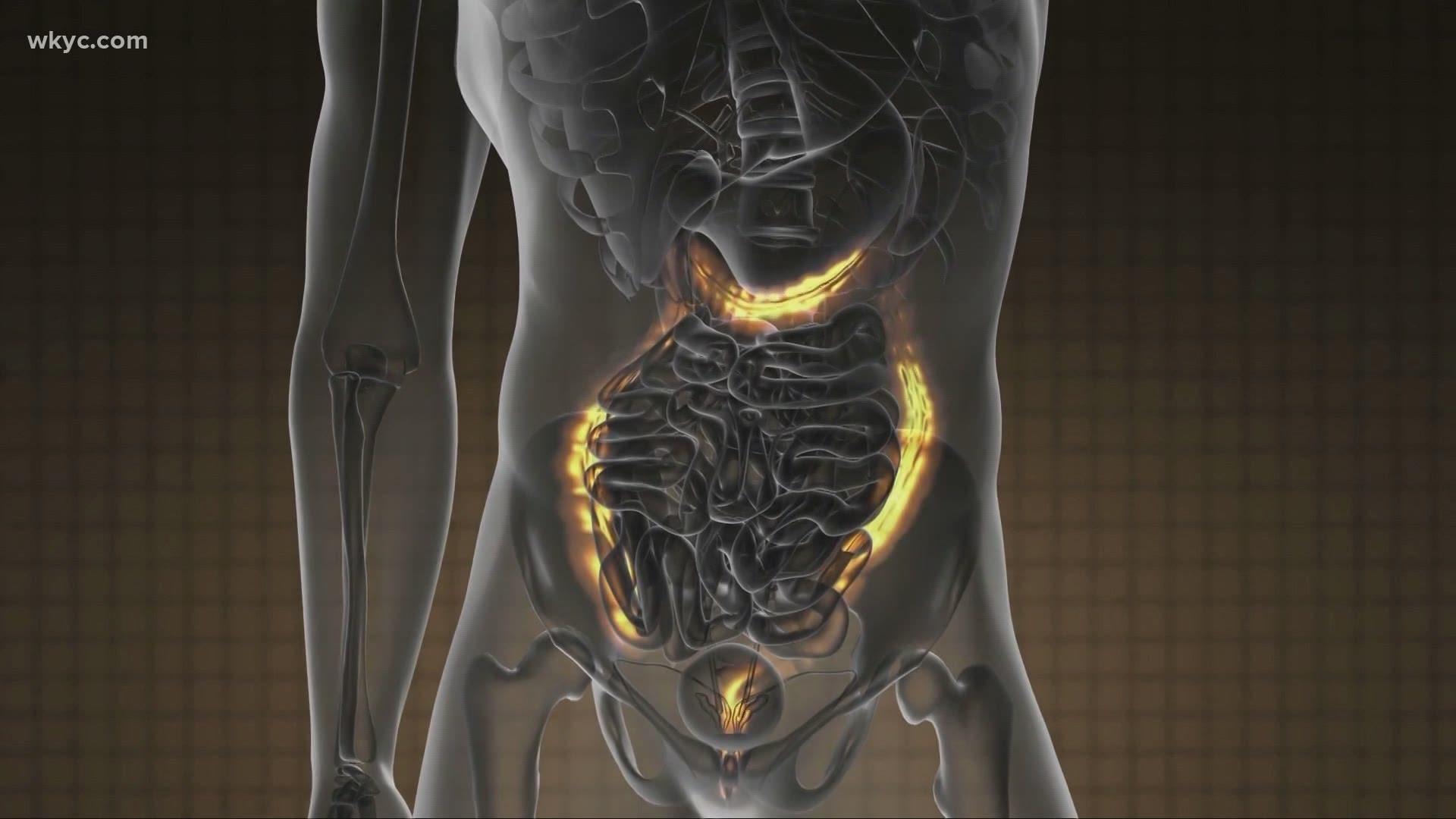
Derek Dystart was the picture of health. He visited his primary care doctor routinely and avoided the illnesses common to black men. But he also never had the test that could have told him there was a deadly cancer growing inside his colon. Even when Dystart went to the emergency room at the age of 21.
“They diagnosed me in the E.R. with gerd, which is kind of like heartburn,” Dystart said. To a 21-year-old, heartburn is often written off as “no big deal.” But still physicians recommended Dystart follow up with a gastrointestinal doctor. Dystart didn’t. After all, he was young and seemingly invincible. Today, more than anything, he wishes he did.
“We don’t think about that as a 21-year-old males and we have blood in our stool, we don’t think about going to see a G.I. doctor,” said Dystart.

Fifteen years of clean physicals, but not a colonoscopy.
Fifteen years, Dystart believes, for his cancer to slowly grow.
“We could have stopped it from getting 15 centimeters big and I do believe that fifteen years correlates with fifteen centimeters,” he asserted.
“We are much less likely to refer people for colonoscopy when they’re younger, I think maybe we should be more so especially for black men,” said Dr. Suneel Kamath, an oncologist with Cleveland Clinic. When Dr. Kamath looked at the National Cancer Database for the last 10 years, a startling set of numbers jumped out.
“About 15% or so of cases in younger patients were in black men. That number was only about 7 or 8% for older patients. So there’s a significantly higher rate in younger patients,” Dr. Kamath pointed out.
On average, black men will have a survivor rate of less than 5 years, a year less than white men, and four years less than Hispanic and Asian men according to Dr. Kamath. And that’s not all:
“These effects didn’t go away, even for black patients who were highly educated, had private insurance, and high incomes as well,” Dr. Kamath said.


“The survival rate is so low because we don’t get diagnosed until too late, because we don’t go to the doctor until the symptoms are deadly,” said Dystart, who urged young men to take symptoms seriously and see a doctor.
Everyone, including young adults, need to take control and pay attention to changes in bowel habits.
“All of us get a little constipated every once in a while, but if it’s gone on for months straight, that’s abnormal,” Dr. Kamath cautioned.
Even more alarming, the majority of young men getting colon cancer have no family history of the disease at all. Ben Simcox was diagnosed at age 38.

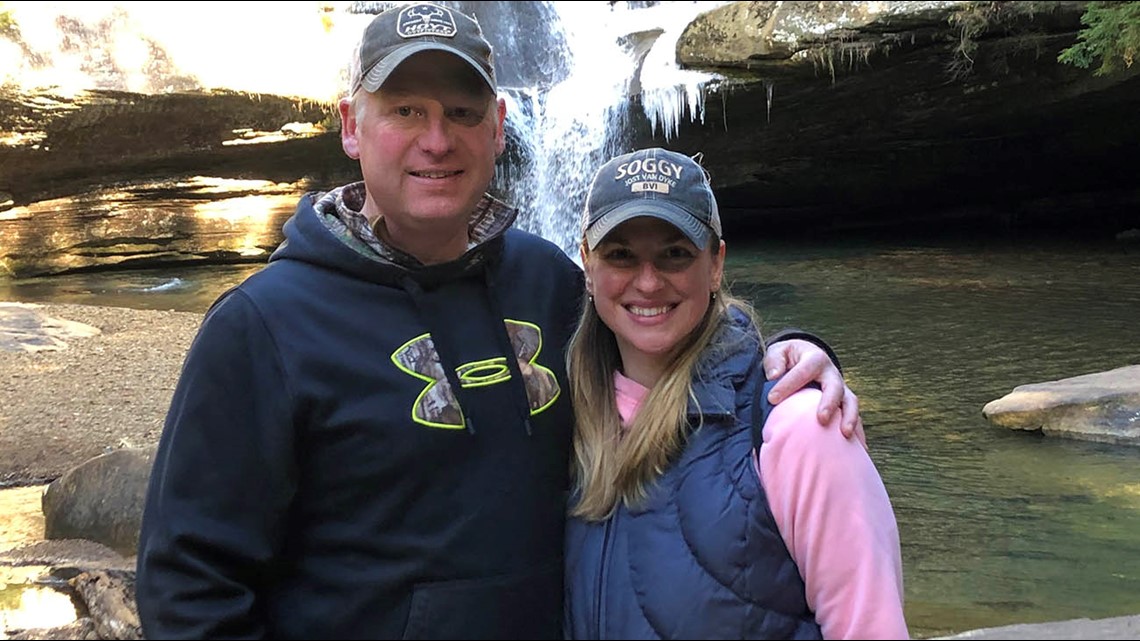
“I looked down and saw a bunch of blood. Obviously, my age, the last thing I was thinking was colon cancer. Instead you just think it might be hemorrhoids,” said Simcox.
His sister pushed Ben to take it seriously. More than likely, he owes her his life. Doctors found cancer.
“If I would have waited 6 months, I would have went in there and there’s nothing they could have done for me,” Simcox said.
Why more young healthy men, with no family history, are getting colon cancer is a mystery.
Diet is one possibility. Eating red meat frequently can increase risk of colon cancer, by nearly 40 percent.
Ben Simcox got the message. He now knows his kids are at risk too.
“I’m cutting way down on pork, red meat, sugar and those types of things. They just aren’t good for you,” he said.
Today, he is doing well and cancer-free.
The road hasn’t been as easy for Derek Dystart. His colon cancer was removed, but he now lives with a colostomy bag. And, the cancer returned. This time it spread to his lungs. But Dystart is fighting. He has too much at stake.
“I have 5 children that I am living for. That’s why I’m fighting this cancer,” he said.
Because being tested is key to prevent, the American Cancer Society released updated screening guidelines in 2018. The new guidelines say that adults at average risk should first be tested at age 45, 5 years younger than the previous recommendations.
The American College of Gastroenterology recommends African-Americans start routine screening at age 45 as they have higher odds of getting colo-rectal cancer than white people. In addition, anyone with an immediate family member, meaning a parent, sibling, or child -- diagnosed before age 60 should be tested at age 40, or 10 years before the age of diagnosis of the youngest relative who had the disease.
Find out more about colostomy surgery at Cleveland Clinic here