COLUMBIA, S.C. — Doctors and engineers in South Carolina created a potentially life-saving ventilator device, which now has FDA approval for emergency use.
A South Carolina emergency room doctor, Sarah Farris, had an idea about how to use a limited amount of ventilators to help more people.
Dr. Farris, a clinical professor of emergency medicine at USC School of Medicine Greenville and Prisma employee, had the idea about three weeks ago.
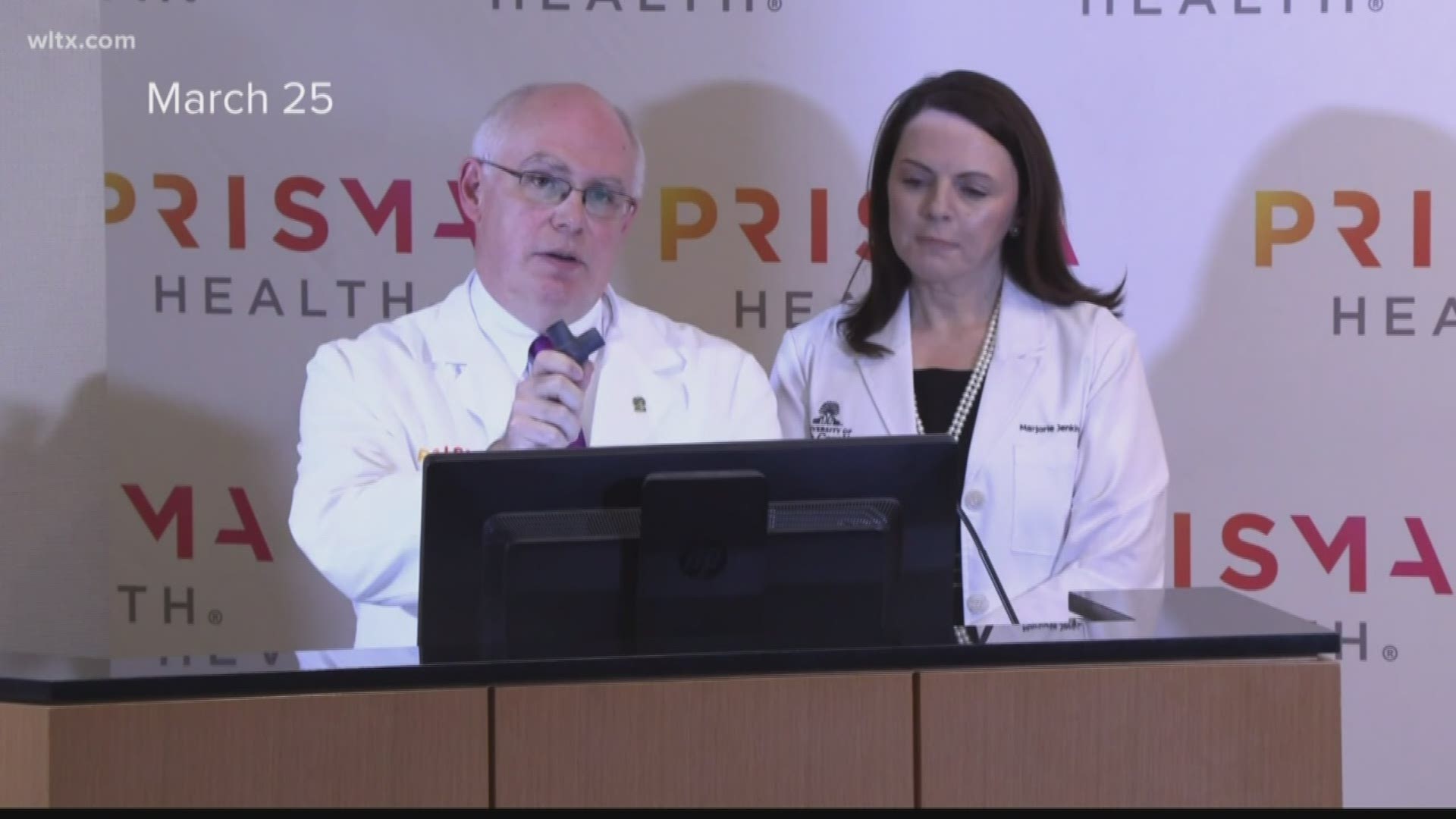
Now, Doctor Marjorie Jenkins, Dean of USC School of Medicine Greenville in coordination with Prisma Health, introduced the potentially life-saving ‘VESper’ device this week.
“If you are out of ventilators, and the issue is to not ventilate someone who needs life-saving support, then the Vesper device will allow you to share a ventilator among patients. The alternative, with this disease, because of the acute respiratory failure that you have, is an almost certain death for that patient,” Jenkins said during a press conference.
VESper allows one ventilator to help up to four patients. VESper is short for ventilator expansion splitter.
Dr. Jenkins, who also serves as Prisma Health’s Chief Academic Officer, has previously worked with the FDA and helped the device get emergency use approval.
Three weeks ago, Dr. Farris had the idea after seeing stories on coronavirus. Eventually, she shared it with her husband, Ryan, whom happens to be a software and biomechanical engineer.
Ryan Farris then wrote a plan on how to 3D-print the device, which he sent to a network of friends and colleagues, whom were able to print it at Clemson. After the first prototype was printed, it was then brought to Prisma Health and USC’s medical experts for testing.
“The device works by attaching to the ventilator in a circuit such that it splits the two circuits out to the patient, we can adjust the ventilatory flow out to the patients to optimize their flow of oxygen, as well as the pressures in which they receive that oxygen,” Dr. Peter Tilkemeier explained.
All told, Dr. Tilkemeier, Prisma Health’s Chair of the Department of Medicine, said roughly 60 people helped develop the device and clinical process for it's use.
“Yeah! Right here in little South Carolina, two weeks, initial thought by an emergency room physician, shared with her husband, then brought forward,” Tilkemeier said over the phone Thursday.
Dr. Jenkins emphasized the rare occurrence the device gained FDA emergency use approval in 72 hours, practically unheard of in normal circumstances.
“They are working 24 hours a day to make this happen. You will never-- I hope never to need or see in my lifetime a 72-hour turnaround for approval from the FDA,” Jenkins said on the same phone call.
Dr. Jenkins reiterated the device is only FDA-approved for emergency situations.
“This is only for those areas that are in greatest need and areas with the potential to exceed their ventilator capacity due to patients affected by COVID-19,” Dr. Tilkemeier added.
Tilkemeier continued, saying Prisma Health currently had no shortage of ventilators.
But the story is different elsewhere, the two medical experts said they've received more than 20 requests from around the world.
Prototypes of the device have already been sent to New York City, New Orleans, and at least one South Carolina hospital.
Before mass production can begin Dr. Jenkins said they need clinical data, stretching at least four hours, from the first patients to use the device. So far, no hospitals have had to use the device on patients.
To access the free printing code, hospitals and companies have to provide proof they have the specialized printers and materials necessary to make the devices.
Dr. Jenkins said Forerunner 3D Printing reached out to her Thursday morning with an offer to print the devices and send them at no cost.