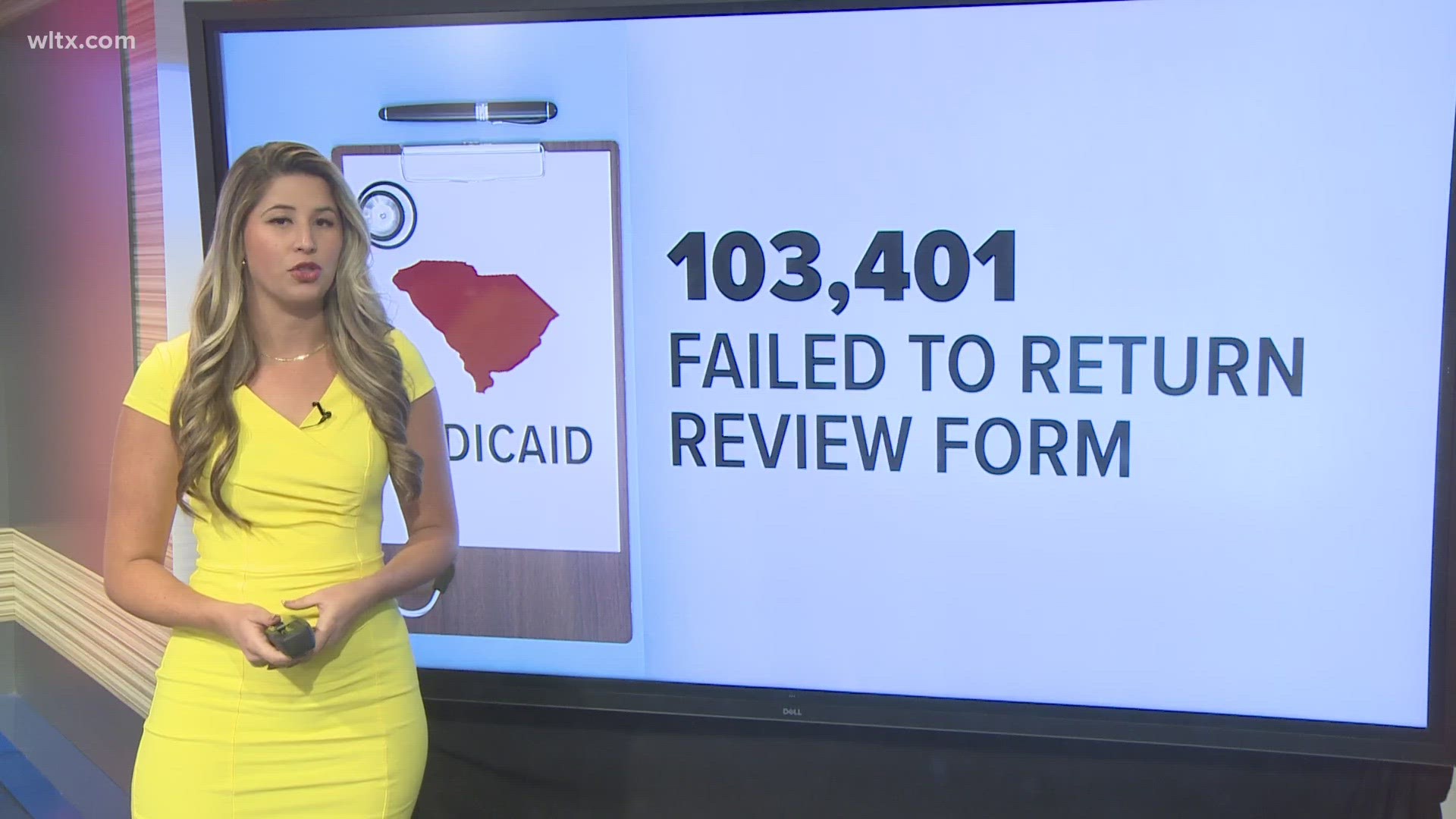
COLUMBIA, S.C. — Medicaid eligibility reviews resumed on April 1, and more than 110,000 South Carolinians have lost Medicaid coverage since that day. Most were because their reviews were not returned to the South Carolina Department of Health and Human Services.
States were prohibited from removing people from Medicaid during the COVID-19 pandemic, but that ban was lifted in April following the declaration of the end of the pandemic.
So far, 228,000 Medicaid members have been reviewed for eligibility. Now nearly 30,000 have had their coverage renewed, 20,000 were renewed automatically with information the agency has on hand, and 6,877 were disenrolled.
Health and Human Services data shows that only 39% of reviews were returned within 60 days or a 90-day grace period. Medicaid recipients are encouraged to ensure the agency has their correct contact information so they don't miss important information about their coverage.