NEW YORK — Although the U.S. outlawed most surprise medical bills starting this year, people who face a health emergency could still find themselves on the hook for hundreds of dollars — or more — in out-of-network fees.
For patients with health insurance, an ambulance ride can set someone back between $500 and $1,000, according to a report from the Public Interest Research Group released Tuesday.
"Ground ambulances are the highest out-of-network biller of all of our health care services," Patricia Kelmar, PIRG's senior director of health care campaigns, told CBS MoneyWatch.
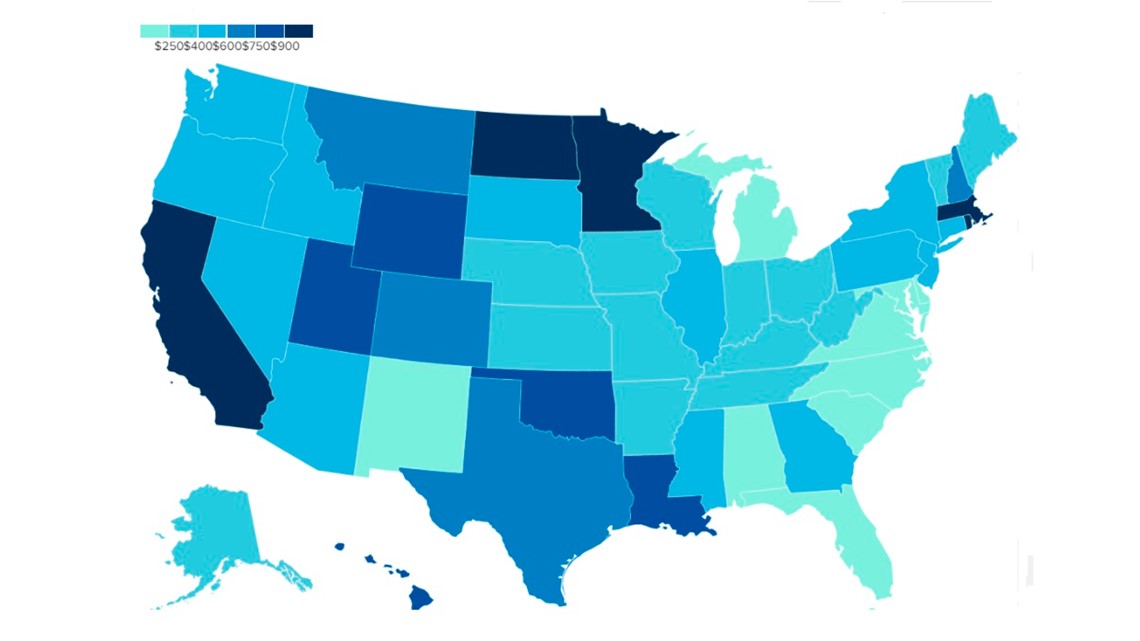
Some 3 million patients go to the hospital in an ambulance each year, more than half of whom will end up with a surprise bill, according to the consumer advocacy group. One study found that between 2010 and 2016, 85% of ambulance patients were hit with a surprise bill for out-of-network services, also known as a balance bill.
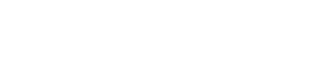
The size of the bill can vary tremendously among states. In Washington, D.C., for example, the median surprise ambulance bill is just $37, according to a study published in Health Affairs in 2020.
By contrast, patients in California, Massachusetts and Minnesota can expect to pay over $1,000 out of pocket for an ambulance ride, after whatever costs their insurance provider covers. In California, the median bill for an ambulance ride is about $1,200, while in Massachusetts it's $1,024 and $1,133 in Minnesota.

Patchwork system
One reason for the disparity in ambulance billing is the proliferation of different types of ambulance services. Modern ambulance networks were established in the 1970s thanks to a major federal push and dedicated funding. But after congressional money dried up in the 1980s, states took over and many programs were cut or privatized, Kelmar said.
"Different communities responded in different ways," she said. "Some municipalities set up funding programs [for ambulance services], some got absorbed into fire departments, some hospitals started ambulance services and private services started up as well."
In recent years, private equity firms have also taken over ambulance services — a change in ownership that often results in aggressive billing and debt collection, PIRG noted. There are about 14,000 different ambulance services around the county, Kaiser Health News has estimated.
Patients are also more likely to be stuck with surprise ambulance bills in certain states. For instance, Maryland bars volunteer ambulances, or those owned by the local government or fire department, from billing patients. Only half of ambulance rides in Maryland result in a surprise bill, according to the Health Affairs study, which looked at patients in a large national health insurance plan.
On the other end of the spectrum, 93% of ambulance rides in Oregon and nearly 90% of those in Washington state result in a surprise bill, the study found.

Altogether, 10 states have laws to limit balance billing for ambulance rides, but even those protections have large gaps. Most notably, they leave out the 60% of insured Americans whose health care is covered by self-funded large insurer plans.
"Roll of the dice"
Unlike a patient who schedules a doctor's visit and can check if those medical services are within their health insurance network, someone calling 911 for a medical emergency has no such ability. Ambulance patients often may not know who operates the transport service.
"You're not going to consult a directory when you're dialing for an ambulance," Kelmar said. "Of course, when you call 911, they're just dispatching the closest available ambulance …. It's a roll of the dice if you'll get that out-of-network bill."
PIRG is pushing Congress to include ambulance bills in the recently passed No Surprises Act, which protects patients in emergency situations from being billed for out-of-network services they didn't agree to. While the law doesn't regulate ambulances, it has directed a committee to study the issue and make recommendations.
"We have figured out how to solve surprise billing with the No Surprises Act. It's working, and people aren't having to face those bills they couldn't avoid. Ground ambulances are the same thing," Kelmar said. "We shouldn't be price-gouging those unlucky few who have an emergency."